You snooze, you lose? Not so much. Sleep dissatisfaction is one of the most prevalent complaints in medical and mental health settings (Ferrie et al., 2011). More than just feeling groggy after a late night out, insomnia is a serious concern for those who aren’t achieving the quantity or quality of sleep they need.
Sleep is essential for our health and has been shown to benefit emotional regulation, physical performance, cognitive processes (e.g., attention, memory, and processing speed), as well as one’s ability to effectively cope with daily stressors (Ellenbogen, 2005 & Vyazovskiy, 2015). Sleep deprivation can lead to significant difficulties with attention, concentration, memory, and decision-making. Not getting enough sleep, or getting low quality sleep, can result in mood disturbances (think irritability, anxiety, and depression), poor physical coordination, and slowed reaction time.
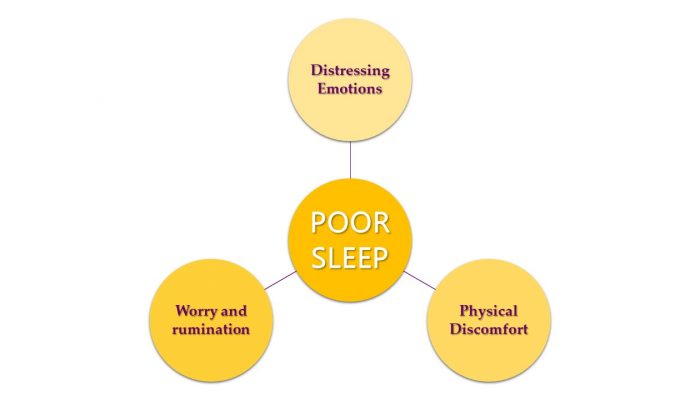
If you are one of millions of people who have difficulty initiating or maintaining sleep, you know that poor sleep is a recipe for disaster when combined with everyday life stress. Your mental health, interpersonal functioning, occupational, and academic performance all suffer when you’re not getting the right amount of z’s. So, what’s keeping you up at night? Science (and experience) tells us that sleep can be negatively impacted by physical discomfort, unhelpful or intrusive thoughts, and distressing emotions.
Everyday life stressors can lead to physical tension, which for some, leads to difficulties relaxing their bodies at night when they get into bed. For those with anxiety, the peace and quiet at bedtime is often interrupted by worries, memories of embarrassing moments, or other obsessive rumination. Similarly, when an individual experiences emotional distress, while it is often “convenient” to push the emotions aside during the day in attempt to check off the to-do list, at night, those emotions can come to the surface and disturb one’s ability to sleep peacefully. And sleeping too much, not enough, or waking earlier than desired in the morning are all common symptoms of depression.
Even in the absence of a diagnosable mental health disorder such as anxiety or depression, poor quality sleep can significantly interfere with your life at home, work, or during leisure. In fact, some of the happiest events in life can lead to poor sleep. Planning a wedding? Welcoming a new baby into your life? Starting a new job? Looking forward to retirement? Changes in your routine and anticipation of exciting life events can get in the way of our sleep and make enjoying those events more difficult.
If you have been experiencing sleep difficulties for more than a few weeks, you may benefit from getting out of your head and into your therapist’s (virtual) office. Cognitive behavioral therapy for insomnia (CBT-I) is a short-term, evidenced-based treatment that Dr. Tomassetti employs to assist her clients in acquiring optimal sleep health. CBT-I has been identified as the first-line intervention for chronic insomnia, with research demonstrating its benefits are superior when compared to individuals being treated with pharmacotherapy (i.e., sleep medications) (Jacobs et al., 2004). Dr. Tomassetti will help you identify sleep habits that would benefit from enhancement to improve your sleep and will assist you in individualizing your bedtime routine by considering your sleep hygiene in the context of your specific environment, preferences, and resources.
Like all CBT approaches, CBT-I begins with assessment and education. Dr. Tomassetti believes it is her job to make YOU your own therapist. To that end, she will teach you effective strategies to employ during the day and prior to bed to promote optimal sleep. Through CBT-I, you will learn a variety of sleep interventions that have been designed in the context of sleep studies and shown to decrease the time it takes to fall asleep, decrease the number of nighttime awakenings, and improve the overall quality of one’s sleep (Newson & Dimitriu, 2020 & Trauer et al., 2015).
CBT-I is highly individualized to meet your needs, and has been proven effective for people of all ages from adolescence to older adulthood (De Bruin et al., 2015 & Irwin, Cole, & Nicassio, 2006). So, whether you are the person planning that three-week trip abroad, or the one ruminating on the embarrassing thing you did five years ago, Dr. Tomassetti will design your treatment accordingly. If you cannot seem to relax physically at night, Dr. Tomassetti will equip you with evidence-based relaxation strategies to soothe your body and mind at night. If it is rumination, worry, or problem-solving the moment your head hits the pillow, then CBT-I will likely include cognitive techniques to help you achieve the inner tranquility you need to drift off at night. If it is the intensity of emotions that prevents you from falling into a peaceful sleep, then Dr. Tomassetti will help you identify emotion regulation strategies to employ throughout the day and at bedtime to address this concern.

Whether you are experiencing temporary life stressors, chronic heightened anxiety, or some other unknown cause of sleep disturbance, CBT-I may be just what you need to get your sleep back on track. Call Dr. Tomassetti today to discuss treatment options and see if CBT-I is the right approach for you.
References
- De Bruin, E. J., Bögels, S. M., Oort, F. J., & Meijer, A. M. (2015). Efficacy of Cognitive Behavioral Therapy for Insomnia in Adolescents: A Randomized Controlled Trial with Internet Therapy, Group Therapy and A Waiting List Condition. Sleep, 38(12), 1913–1926. https://doi.org/10.5665/sleep.5240
- Ellenbogen, J. M. (2005). Cognitive benefits of sleep and their loss due to sleep deprivation. Neurology, 64(7), 25-27.
- Ferrie, J. E., Kumari, M., Salo, P., Singh-Manoux, A., & Kivimäki, M. (2011). Sleep epidemiology—a rapidly growing field. International Journal of Epidemiology, 40(6). 1431–1437.
- Irwin, M. R., Cole, J. C., Nicassio, P. M. (2006). Comparative meta-analysis of behavioral interventions for insomnia and their efficacy in middle-aged adults and in older adults 55+ years of age. Health Psychology, 25(1). 3–14.
- Jacobs, G. D., Pace-Schott, E. F., Stickgold, R., & Otto, M. W. (2004). Cognitive behavior therapy and pharmacotherapy for insomnia: A randomized controlled trial and direct comparison. Arch Internal Medicine, 164(17). 1888–1896. doi:10.1001/archinte.164.17.1888
- Newsom, R. & Dimitriu, A. (2020). Cognitive behavioral therapy for insomnia (CBT-I). Sleep foundation.
- Trauer, J. M., Qian, M. Y., Doyle, J. S., Rajaratnam, S. M., & Cunnington, D. (2015). Cognitive Behavioral Therapy for Chronic Insomnia: A Systematic Review and Meta-analysis. Annals of internal medicine, 163(3), 191–204. https://doi.org/10.7326/M14-2841
- Vyazovskiy V. V. (2015). Sleep, recovery, and metaregulation: explaining the benefits of sleep. Nature and science of sleep, 7, 171–184. https://doi.org/10.2147/NSS.S54036
